Background:
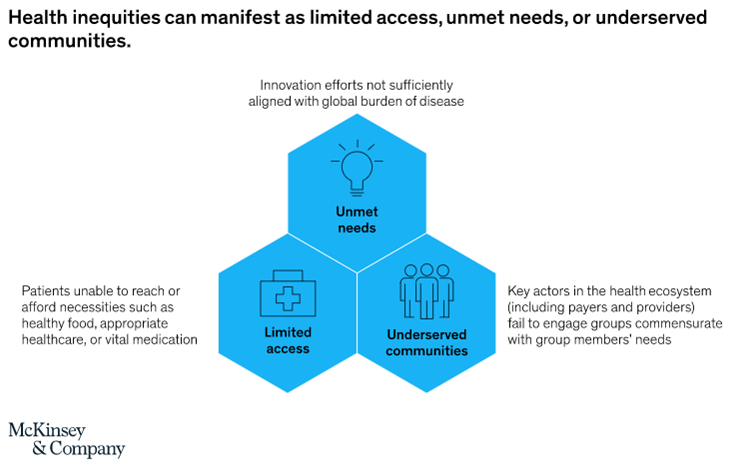
Patient access schemes are innovative pricing agreements proposed by pharmaceutical companies to improve cost-effectiveness and enable patients to gain access to high cost drugs and treatments[1]. Other than pricing, patient access schemes can look into addressing other gaps in healthcare service delivery that are hindrances for patients in receiving the care they need. Some of these as outlined by McKinsey & Co. include unmet needs, underserved communities and limited access as described in the figure below[2].
Patient access programs serve varied purposes depending on the organizations that front them and this is the basis for which we have different models. Governments with a responsibility to provide healthcare services as a social responsibility designs access programs including public health insurances schemes to support with financing of healthcare services in various communities. For non-governmental organizations that provide health services through medical outreach programs and standing health programs, such services are aligned to their mission. Biopharmaceutical companies have also been involved in patient access programs with a mission of improving access to their medicines and medical technologies to individuals who would otherwise be unable to use these products and services.
The basic principle for patient access programs is therefore to improve access to lifesaving healthcare products and solutions to patient who need them to improve their health status or keep them healthy.
Essentials of a Robust Patient Access Program:
A robust patient access program capable of delivering on its mandate needs strategic, deliberate and structured design informed by a deep contextual assessment of variables i.e.
- Patient Access Gap Assessment: Regardless of the entity working responsible for the design of a patient access program, there is need to establish the need. Clarity on the gap in access to healthcare services is critical in ascertaining market-fit of the solution. This also covers for the contextual assessment to establish which priority to focus on e.g., if dealing with a community where the burden of Malaria is substantially high based on epidemiological data designing a care program for malaria may not be the best solution. It is important to find out the gaps in care for malaria which could be preventative measures i.e., lack of mosquito treated nets or even environmental risks such as mines which serve as water reserves & incubators for mosquito larvae, diagnostic or access to medicines. With a clear understanding of the gap in care it’s easier to design a project that will serve these needs. An example of this was documented in Visceral Leishmania management in Kitui County, Kenya where the clinical suspicion was low with most patients being referred for specialized care, being screened for cancers and delaying treatment. In such a case the best approach to build capacity for clinicians to be able to diagnose early and initiate treatment when needed[3].
- Clarity on Patient Decision Journey & Healthcare Service Models: Patient access programs are designed to improve access for patients through healthcare systems. There is therefore a need to understand the patient decision journey across the care continuum i.e., At what point does our case patient (patient whose need we intend to address) interface with the healthcare system? What is the entry point to the healthcare system for the patient? What influences these decisions for this patient? Which healthcare service models exist for this patient? Which of these is high priority in reaching him/her? This understanding is important in helping the design of the program to meet the patient where they are optimally.
- Clarity on internal capabilities & strengths: Before venturing out to design a patient access program every entity must acknowledge their limitations and inability to solve all the problems. They need to focus on their core capabilities which may be drawn from their business models i.e. a pharmaceutical company would focus on medicines production and ensuring access to these medicines considering it is within their line of expertise. Additional requirements could be sourced from other entities either through strategic partnerships or services at a fees.
- Stakeholder Knowledge: In designing a patient access programs, entities need to acknowledge that often times they are not the first people to see the gap and set out to address it. They should therefore focus on mapping stakeholders already working on this particular problem or with an interest in it with specific attention on what their probable or perceived role could be. This helps create synergies, improve efficient use of available resources and most importantly set sustainability frameworks for the program.
- Strategic alignment on company offering, patient needs and access pillars: There is need for a strategic & operational alignment in the needs, organizational capabilities and the specific access strategy to be deployed. A misalignment not only wastes resources but gives false hope to the intended recipients derailing probable positive advances.
- Project Design: With clear understanding of the needs, stakeholder landscape, internal capabilities and offerings for the patient access program, the team can then venture into actual design of the patient access program to deliver on the mission adopting project management principles along the way.
Experiences from the field:
In October 2020, we started work in our first patient access program to improve access to care for patients living with diabetes and hypertension in Kasarani Sub-County, domiciled within Kasarani Health Center[4]. This was a journey defined by experiences, observations and existing community goodwill & support. In this explorative reflection, we share insights on the process and some lessons which are worth adoption in future patient access programs.
During his internship at Kasarani Health Center, our Co-founder noted a gap in access to care for patients living with diabetes. When patients finished their consultation with clinicians at the hospital, they would come to the pharmacy with prescriptions for medicines they needed. Unfortunately, less that 30% of the prescriptions for diabetes and hypertension could be filled. Patients were accustomed to being asked to buy medicines from neighboring pharmacies which was noted to be contributing to the decline in their visits where additional services such as monitoring of vitals, counselling and medication therapy reviews could be conducted. This was negatively impacting the quality of care for these patients. Being on the backdrop of COVID-19 with heightened risk to this population, they need extra care and attention both in addressing the psychosocial problems they were experiencing and in managing their conditions.
To close the gaps, we consulted with the Clinician-In-Charge who was open to the suggestion of having a program for these patients and luckily there was already a partner keen to support with establishment of a patient support group (special purpose vehicle for the program). The program was designed as a patient support group which was registered and an account opened for them with Mission for Essential Drugs (MEDS). Leveraging on our technical expertise, we focused on health education, patient counselling, medication reconciliation and therapy monitoring. Patients would have to pay Kshs. 500 per month which would be used to buy the required medicines and each patient was then assured of receiving their medicines thus promoting access and compliance to care. The clinic having three (3) clinicians, were willing to dedicate one clinician to coordinate the clinic days which were once a month to offer clinical services.
Through the formative six (6) months of the program before transitioning, we had enrolled 43 patients to the program who were assured of continuously receiving their monthly refill of medications over this period, getting clinical counsel and additional health education when and where necessary as per the talking points decided on by themselves. The program got patients mostly elderly people talking about stress and mental health which is an uncommon occurrence[5]. Patients who needed specialized care could be referred to Mama Lucy Kibaki Hospital or Kenyatta National Hospital (KNH) establishing a robust referral pathway for patients when needed.
Insights & Best Practices
- An understanding of patients’ pain-points serve as a critical tool in helping them on their journey to care. By optimizing their pain point on accessing medicines which they consider critical for the management of their conditions, they were able to come to the clinic reliably for follow up care.
- Understanding the care continuum is an imperative for a successful patient access program. Being able to deliver healthcare services across the spectrum i.e., health promotion, disease management and ancillary services when needed by patients makes them inclined to engage more and improve the outcome of their care.
- Structured stakeholder engagement is an essential component in design and implementation of a successful patient access program. Kasarani Health Center as a host organization was the anchor for the patient support group, PharmAccess Foundation (M-TIBA) was able to support with the registration of the patient support group, MEDS was able to supply medicines as per the needs and we were able to run the health programs within our capability areas.
- Transparency at the get go with each stakeholder is a critical component in ensuring the program gains stability to serve the patients who are dependent on them for their health outcomes. By being clear and transparent on what our capabilities were, patients were able to engage proactively and deliver on their end through the monthly contributions in purchase of their medicines.
Challenges Experienced
The program experienced some challenges like every other program which are critical for consideration in any future programs of the same nature:
- Patient access programs need reliable resourcing to be sustainable. Financing gaps especially for the operational expenses led to decline in support for the program from the teams who were volunteering their time. This became critical where other conflicting opportunities came up where they could earn a living wage.
- Workforce shortfalls at the facility i.e., with 3 clinicians, when one was supporting the clinic days, the other core operations of the hospital were negatively impacted putting a strain on the program.
About:
Ryculture Health and Social Innovation is a forward looking social enterprise committed to improving access to quality healthcare service and promoting human capital development through health research, health communication, health systems strengthening and human capacity development.
Our aspiration is to contribute to the edification of our societies towards a socially responsible, healthy and prosperous generation.
Project Background:
This project was part of our health systems strengthening programs under our Non-Communicable Diseases (NCDs) Program.
Report written by: Dr Odhiambo David
For more information, contact us through email: info.ryculture@gmail.com
You can download the PDF here.
[1] Patient Access Scheme Liaison Unit, National Institute for Health and Care Excellence: https://www.nice.org.uk/about/what-we-do/patient-access-schemes-liaison-unit
[2] Health equity: A framework for the epidemiology of care: https://www.mckinsey.com/industries/life-sciences/our-insights/health-equity-a-framework-for-the-epidemiology-of-care
[3] Neglected Tropical Diseases (NTDs): Should we literally neglect them? (Case for Leishmaniasis in Kitui County, Kenya): https://www.linkedin.com/pulse/neglected-tropical-diseases-ntds-should-we-literally-neglect-david/
[4] Launch of the Kasarani Health Center NCDs Clinic – 9th October 2020: https://ryculture.org/launch-of-the-kasarani-health-center-ncds-clinic-9th-october-2020/
[5] Health education on stress management to diabetic and hypertensive patients at the NCDs clinic at Kasarani Health Centre: https://ryculture.org/health-education-on-stress-management-to-diabetic-and-hypertensive-patients-at-the-ncds-clinic-at-kasarani-health-centre-13th-november-2020/

