In an era where the world’s attention is often riveted on infectious diseases and pandemics, there exists a silent and relentless global epidemic known as Non-Communicable Diseases (NCDs)[1]. These are a group of medical conditions that do not owe their origins to infectious agents like bacteria or viruses, and they cannot be passed from person to person. NCDs tend to develop insidiously over extended periods, their emergence closely tied to factors such as genetics, lifestyle choices, and environmental influences. The four primary categories of NCDs encompass:
- Cardiovascular diseases: These encompass heart diseases and strokes, often linked to factors like high blood pressure, high cholesterol, smoking, and unhealthy diets.
- Diabetes: A metabolic disorder characterized by elevated blood sugar levels, often related to genetics, obesity, and lifestyle choices.
- Cancer: The uncontrollable growth of abnormal cells in the body with various types and risk factors, including genetics, exposure to carcinogens, and lifestyle factors.
- Chronic Respiratory Diseases: These include conditions like chronic obstructive pulmonary disease (COPD) and asthma, often associated with smoking, air pollution, and occupational exposures.
Beyond these commonly recognized NCDs lie an array of other health conditions, including Chronic Kidney Disease (CKD), neurological disorders like Alzheimer’s and Parkinson’s, and mental health disorders such as depression and substance abuse. Collectively, these diseases constitute a formidable global health concern, accounting for a significant share of illness, disability, and premature death worldwide. Their chronic nature necessitates ongoing management and care, leading to high healthcare costs, diminished workforce productivity, and financial insecurity for affected individuals.
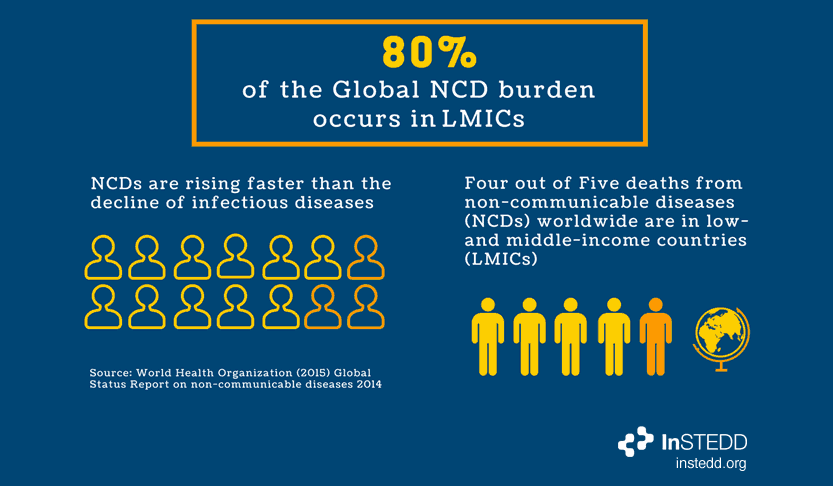
While NCDs may not discriminate, healthcare systems often do, resulting in stark disparities in health outcomes and overall well-being. These disparities manifest along socioeconomic, geographic, cultural, and ethnic lines, as well as within healthcare systems marked by inefficiencies and resource imbalances. As NCD-related deaths surpass those caused by communicable diseases, it is imperative that we delve into the unequal battle against NCDs and explore avenues for equitable care and prevention.
The Unequal Battle
Access to quality healthcare services for individuals battling NCDs is far from equal, creating stark disparities in outcomes and well-being. Healthcare disparities manifest in several ways:
- Socioeconomic status: Individuals with lower socioeconomic status often face barriers in obtaining timely and comprehensive care.
- Geographic location: Urban areas often boast better healthcare infrastructure compared to underserved rural regions, limiting the reach of essential NCD services.
- Cultural and Ethnic factors: These factors, along with distrust of healthcare systems, can hinder individuals from certain ethnic backgrounds in seeking and receiving appropriate care. Understanding cultural nuances is crucial for providing inclusive healthcare.
- Healthcare System Inefficiencies: Inefficiencies, long waiting times due to a lack of enough healthcare professionals, and unequal resource distribution exacerbate disparities within the healthcare system.
Deaths from NCDs now exceed all communicable disease deaths combined, claiming 7 out of 10 lives worldwide. In Kenya, NCDs are responsible for over 50% of in-patient hospital admissions and 39% of all annual deaths. Cardiovascular diseases account for the majority of NCD-related deaths in the country. Changing social, economic, and structural factors have fueled this crisis. Urbanization and the spread of unhealthy lifestyles such as smoking, excessive alcohol intake, and an unhealthy diet have contributed to the NCD crisis that prematurely claims 15 million lives annually, mostly before the age of 70.[2]
NCDs place continuous social and economic strain on households due to their long-term management. Poor and vulnerable populations bear the brunt of expensive NCD management, with limited health insurance coverage and catastrophic health expenditure.
The Ripple Effects of NCDs
The effects of NCDs extend beyond the individual diagnosed with the condition. NCDs often come with emotional burdens, causing stress, anxiety, and depression not only for the affected individual but also for family members.[3] Witnessing a loved one’s struggle with a chronic condition can be emotionally draining. The cost associated with NCDs, including medical expenses and lifestyle changes, can place a significant financial burden on families, leading to financial instability or even bankruptcy.
Family members often become caregivers for individuals with NCDs, a demanding role that requires time and effort for daily care, medical appointments, and emotional support. NCDs can lead to absenteeism from work due to illness or caregiving responsibilities, resulting in reduced household income and economic strain on the community. Within the context of community resources, NCDs place demands on local healthcare systems, affecting resource allocation. An increase in NCD cases can strain healthcare facilities and lead to longer wait times for all patients, especially in already strained systems due to a lack of adequate healthcare workers and resources.
NCDs often coexist with other health conditions, creating a complex web of healthcare needs within a family or community. Managing multiple health conditions can be overwhelming. It is crucial to recognize that NCDs are not isolated health issues but have far-reaching consequences that affect the social, economic, and emotional fabric of families and communities. Addressing NCDs requires a holistic approach that considers these ripple effects and works toward comprehensive solutions for prevention, management, and support.
In the Face of NCDs: A Call for Holistic Action
The omnipresent threat of Non-Communicable Diseases casts a shadow that stretches far beyond individual health. It infiltrates the very fabric of our families, communities, and societies, introducing emotional burdens, financial strains, and caregiving responsibilities that reverberate throughout the lives of countless individuals. While these diseases relentlessly claim lives, the toll extends to loved ones who bear witness to the relentless struggle against chronic conditions.
In addition to the emotional turmoil, NCDs precipitate a cascade of economic repercussions, from skyrocketing medical expenses to diminished household incomes due to absenteeism from work. Communities are not spared either, as strained healthcare systems struggle to cope with the surge in NCD cases, leading to longer waiting times for all patients.
Recognizing that NCDs seldom exist in isolation, but rather in complex clusters with other health conditions, it is evident that a comprehensive approach is the only viable path forward. We must address NCDs as interconnected health issues with far-reaching consequences. This approach calls for a multifaceted strategy that encompasses prevention, management, and support, while also prioritizing equity in healthcare access.
As NCDs continue to exact a heavy toll on individuals, families, and communities, it is our collective responsibility to champion holistic solutions that empower individuals to lead healthier lives, reduce the socioeconomic disparities associated with these diseases, and ensure that the ripple effects of NCDs no longer define the health and well-being of our global community. In the face of this silent epidemic, we must unite in our resolve to provide comprehensive care, support, and hope for a healthier future.
References
[1] Non-Communicable Diseases https://www.who.int/news-room/fact-sheets/detail/noncommunicable-disease
[2] Non-Communicable Disease Program https://www.kemri.go.ke/non-communicable-diseases-ncd-program
[3] Global Burden of Disease Collaborative Network, Global Burden of Disease Study 2019 (GBD 2019) Results (2020, Institute for Health Metrics and Evaluation – IHME) https://vizhub.healthdata.org/gbd-results/
Article authored by Dr. Terry Kuria, Pharmacist & Member Ryculture YouTH Voices Network